Choosing the right imaging for your patients can make or break your treatment outcomes. Dental professionals face this CBCT vs conventional radiographs decision daily, and getting it wrong wastes money and potentially compromises patient care.
This guide helps dentists, oral surgeons, and dental teams make smarter dental imaging decision making choices based on clinical need, cost, and diagnostic value. You’ll discover when cone beam CT imaging gives you the edge over traditional X-rays, and when conventional X-ray benefits still win the day.
We’ll break down the clinical scenarios where CBCT delivers game-changing 3D detail for complex cases like implant planning and endodontics. You’ll also learn when conventional radiographs remain your best bet for routine diagnostics and cost effective dental imaging. Finally, we’ll walk through a practical cost-benefit analysis that helps different practice settings choose the right imaging approach for their patients and budget.
Understanding CBCT Technology and Its Core Advantages

Three-dimensional imaging capabilities for comprehensive diagnosis
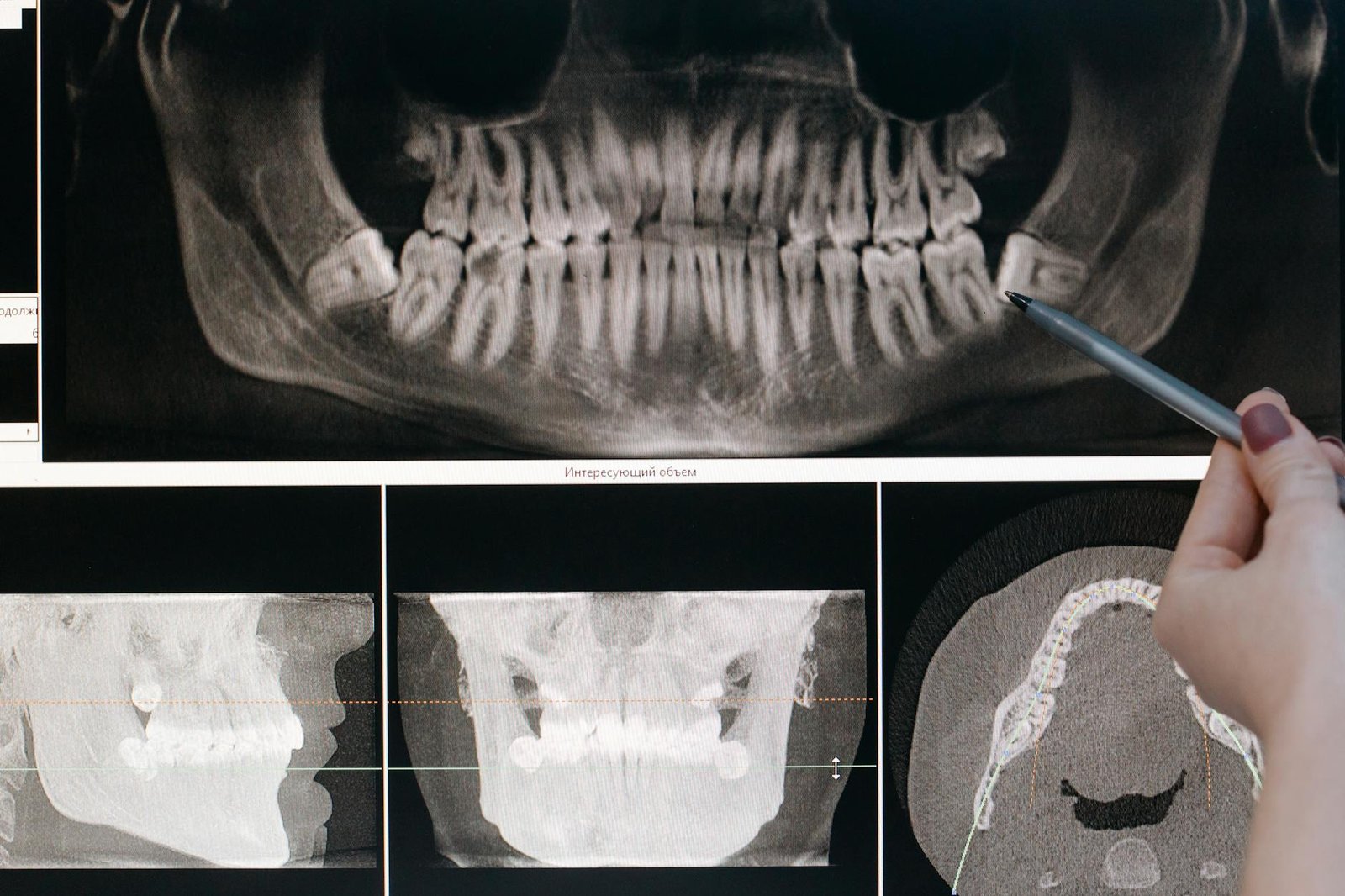
Cone beam CT imaging transforms the way dental professionals approach diagnosis by delivering complete three-dimensional visualization of oral and maxillofacial structures. Unlike conventional radiographs that compress anatomical structures into flat, two-dimensional images, CBCT provides volumetric data that can be manipulated and viewed from multiple angles and planes.
The technology works by rotating a cone-shaped X-ray beam around the patient’s head, capturing hundreds of individual projection images during a single scan. These images are then reconstructed by sophisticated software algorithms to create detailed cross-sectional views in axial, sagittal, and coronal planes. This comprehensive approach allows practitioners to examine structures that might be obscured or overlapped in traditional radiographic images.
CBCT’s three-dimensional capabilities prove especially valuable when diagnosing complex cases involving impacted teeth, root morphology variations, and anatomical anomalies. The technology reveals the exact position of impacted third molars relative to the inferior alveolar nerve, mandibular canal, and adjacent tooth roots with precision that conventional X-rays simply cannot match. This level of detail helps prevent complications during surgical extractions and guides treatment planning decisions.
Root canal therapy benefits significantly from CBCT’s dimensional imaging. The technology identifies additional canals, calcifications, and anatomical variations that traditional periapical radiographs might miss. Studies show that CBCT detects up to 40% more root canals compared to conventional radiographic methods, leading to more successful endodontic outcomes.
Periodontal diagnosis gains new dimensions with CBCT technology. The imaging modality reveals bone defects, furcation involvement, and periodontal ligament space changes in three dimensions. This comprehensive view helps distinguish between different types of periodontal defects and guides regenerative treatment approaches more effectively than traditional radiographs.
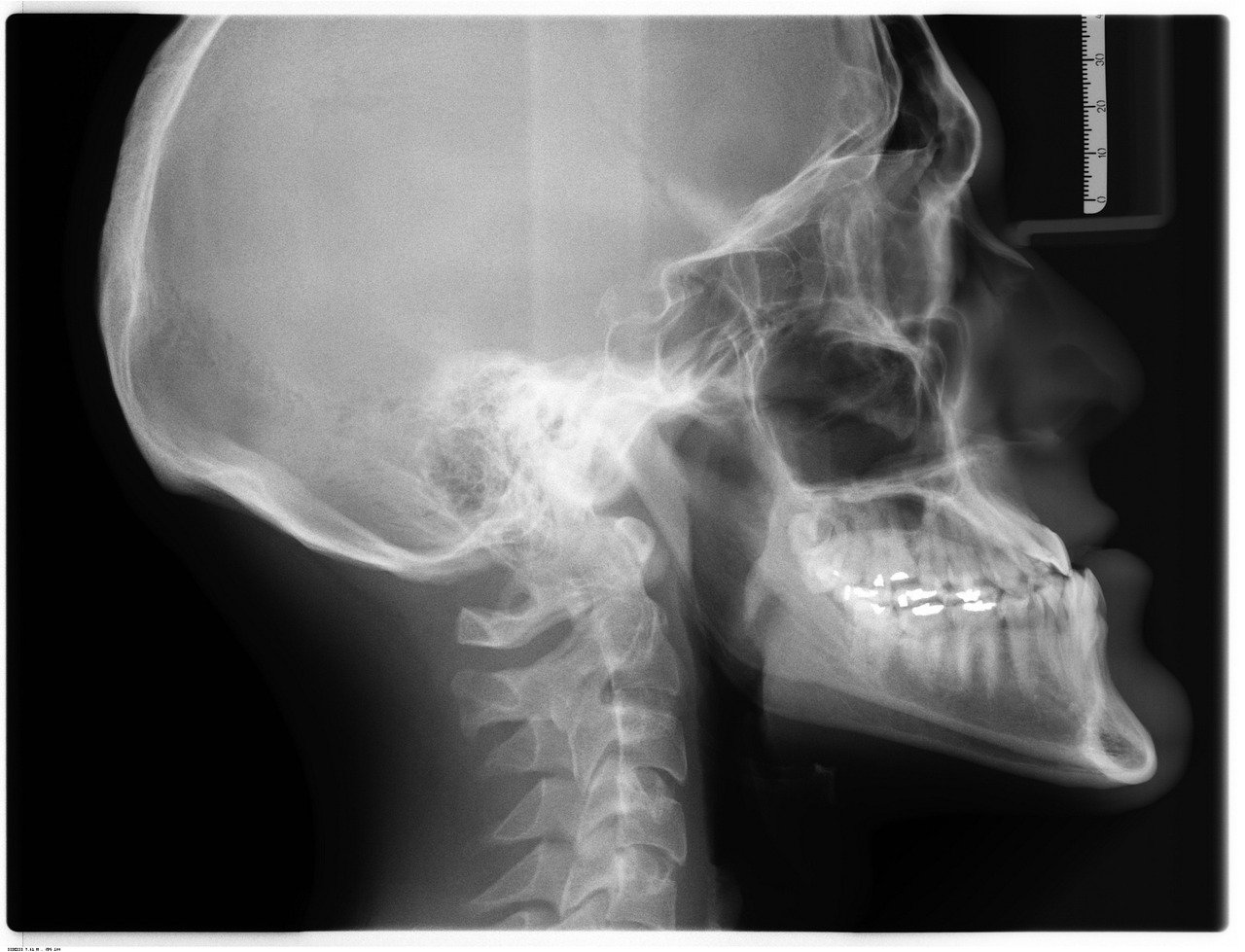
The three-dimensional aspect also revolutionizes orthodontic diagnosis and treatment planning. CBCT provides detailed information about tooth root positions, bone thickness, and anatomical limitations that influence tooth movement. Orthodontists can visualize the entire dentofacial complex and plan treatments with greater precision, especially for complex cases involving impacted teeth or skeletal discrepancies.
Enhanced spatial resolution for detailed anatomical visualization
CBCT technology delivers exceptional spatial resolution, typically ranging from 0.1 to 0.4 millimeters, which surpasses most conventional radiographic systems. This enhanced resolution capability allows dental professionals to visualize minute anatomical details that remain invisible on traditional X-rays.
The superior spatial resolution becomes particularly important when examining fine anatomical structures like the lamina dura, periodontal ligament space, and cortical bone boundaries. These structures appear as distinct, well-defined entities on CBCT images, whereas conventional radiographs often show them as blurred or overlapping features due to anatomical superimposition.
Endodontic applications showcase CBCT’s resolution advantages most clearly. The technology identifies microscopic root fractures, lateral canals, and apical anatomy variations with remarkable clarity. Root fractures that measure less than 0.2mm in width become visible on high-resolution CBCT scans, while conventional periapical radiographs might miss these critical findings entirely. This enhanced detection capability directly impacts treatment success rates and long-term prognosis.
Implant planning benefits tremendously from CBCT’s spatial resolution capabilities. The technology provides precise measurements of available bone width, height, and density at potential implant sites. Practitioners can evaluate bone quality, identify anatomical structures like the mandibular canal and maxillary sinus, and plan optimal implant positioning with sub-millimeter accuracy. This level of precision reduces surgical complications and improves implant success rates.
The enhanced resolution also proves valuable for detecting early pathological changes. Small cysts, granulomas, and bone lesions become visible before they would appear on conventional radiographs. Early detection allows for timely intervention and often less invasive treatment approaches, benefiting both patient outcomes and practice efficiency.
Temporomandibular joint evaluation represents another area where CBCT’s spatial resolution provides significant advantages. The technology reveals detailed joint anatomy, including condylar morphology, joint space dimensions, and early degenerative changes that conventional TMJ radiographs might miss. This detailed visualization helps clinicians make accurate diagnoses and develop appropriate treatment plans for TMJ disorders.
Reduced radiation exposure compared to medical CT scans
CBCT technology offers a compelling radiation safety profile when compared to conventional medical CT scans, making it more suitable for routine dental applications. The effective radiation dose for a typical dental CBCT scan ranges from 30 to 300 microsieverts, significantly lower than medical CT scans which can deliver doses of 2,000 to 10,000 microsieverts depending on the examination type.
This dose reduction stems from several technological advantages inherent in CBCT design. The cone-shaped beam geometry allows for more efficient X-ray utilization compared to the fan-shaped beams used in medical CT scanners. The focused beam pattern reduces scatter radiation and limits exposure to the specific area of interest, minimizing radiation to surrounding tissues.
CBCT scanners also employ pulsed X-ray exposure techniques rather than continuous radiation delivery. The system only activates the X-ray source when needed for image acquisition, reducing total exposure time and cumulative radiation dose. Modern CBCT units incorporate automatic exposure control systems that adjust radiation parameters based on patient size and anatomical density, optimizing image quality while minimizing dose.
The radiation dose comparison becomes even more favorable when considering CBCT versus conventional radiographic series. A full mouth series of periapical and bitewing radiographs delivers approximately 150 microsieverts of radiation, while a limited-field CBCT scan covering the same diagnostic area typically requires 50-100 microsieverts. This means CBCT can provide superior three-dimensional information at radiation levels comparable to or lower than conventional radiographic examinations.
Field of view optimization plays a crucial role in CBCT’s radiation efficiency. Modern units allow practitioners to select specific volumes of interest, from single-tooth regions to full maxillofacial coverage. Smaller field sizes dramatically reduce radiation exposure while still providing necessary diagnostic information. A single-tooth CBCT scan may deliver as little as 10-30 microsieverts, comparable to a single periapical radiograph.
Patient positioning and collimation technologies further enhance radiation safety in CBCT systems. Lead aprons and thyroid collars remain important protective measures, while newer systems incorporate additional filtration and beam-hardening techniques that reduce soft tissue exposure without compromising image quality.
Real-time cross-sectional views for accurate treatment planning
CBCT’s ability to generate real-time cross-sectional views revolutionizes treatment planning accuracy across multiple dental specialties. The technology provides immediate access to axial, sagittal, and coronal sections, allowing practitioners to evaluate anatomical relationships and pathological conditions from multiple perspectives during patient consultations.
Implant treatment planning exemplifies CBCT’s real-time advantages most dramatically. Practitioners can measure bone dimensions, evaluate bone quality, and identify critical anatomical structures like the inferior alveolar nerve or maxillary sinus in real-time during the planning session. Interactive software allows for virtual implant placement, enabling clinicians to optimize positioning, angulation, and depth before surgery begins. This real-time capability reduces surgical time, improves outcomes, and enhances patient confidence through visual treatment presentations.
Endodontic treatment planning benefits significantly from CBCT’s cross-sectional imaging capabilities. Real-time evaluation of root canal anatomy reveals complex morphology, calcifications, and anatomical variations that influence treatment approaches. Practitioners can assess the three-dimensional relationship between roots and anatomical structures, identify additional canals, and plan access cavity preparations with greater precision.
Orthognathic surgery planning represents another area where CBCT’s real-time cross-sectional views provide substantial advantages. Surgeons can evaluate skeletal relationships, measure bone dimensions, and plan osteotomy locations with unprecedented accuracy. The ability to visualize hard and soft tissue relationships in three dimensions during the planning session improves surgical outcomes and reduces operative time.
Periodontal treatment planning gains new dimensions through CBCT’s cross-sectional imaging capabilities. Real-time evaluation of bone defects, furcation involvement, and anatomical variations guides regenerative treatment approaches. Practitioners can assess the three-dimensional morphology of periodontal defects and select appropriate regenerative materials and techniques based on precise anatomical measurements.
The real-time aspect also enhances patient communication and case acceptance. Visual presentation of three-dimensional anatomy helps patients understand their conditions and proposed treatments more clearly. Interactive manipulation of cross-sectional views during consultations improves patient engagement and facilitates informed consent processes.
Modern CBCT software platforms provide advanced visualization tools that enhance real-time treatment planning capabilities. Multi-planar reconstruction, volume rendering, and curved planar reformation techniques allow practitioners to customize image presentations based on specific diagnostic needs. These tools enable rapid assessment of complex anatomical relationships and support more accurate treatment planning decisions.
Integration with computer-aided design and manufacturing systems further amplifies CBCT’s real-time planning advantages. DICOM data from CBCT scans can be directly imported into surgical planning software, enabling the design of surgical guides and prosthetic components based on actual patient anatomy. This seamless workflow reduces planning time and improves treatment precision across multiple disciplines.
Conventional Radiographs: Proven Benefits and Applications
Cost-effective solution for routine dental examinations
Conventional radiographs remain the backbone of dental imaging for good reason – they deliver exceptional value when it comes to routine diagnostic needs. When you’re running a busy dental practice, the economics matter just as much as the clinical outcomes. Traditional X-rays cost significantly less to acquire and operate compared to CBCT systems, making them the smart choice for everyday dental examinations.
The initial investment for conventional radiographic equipment ranges from $15,000 to $40,000 for a complete digital setup, while CBCT machines typically start around $150,000 and can exceed $400,000 for high-end units. This dramatic cost difference means practices can allocate their resources more effectively, investing in other essential equipment or staff training while still maintaining excellent diagnostic capabilities.
Operating costs tell a similar story. Conventional X-ray systems consume minimal electricity, require less specialized maintenance, and have lower insurance premiums. The maintenance contracts for traditional radiographic equipment typically run $2,000-$5,000 annually, compared to $15,000-$25,000 for CBCT systems. These ongoing expenses add up quickly over the lifespan of the equipment.
For routine examinations like bitewing radiographs, periapical films, and panoramic images, conventional radiographs provide all the diagnostic information needed at a fraction of the cost. A standard bitewing series can detect interproximal caries, evaluate bone levels around teeth, and assess restoration integrity with remarkable clarity. The diagnostic yield from these cost-effective images makes them invaluable for preventive care and treatment planning for common dental conditions.
Insurance reimbursement patterns also favor conventional radiographs for routine procedures. Most dental insurance plans readily cover standard X-rays as part of regular examinations, while CBCT imaging often requires pre-authorization and may face coverage limitations. This reimbursement structure makes conventional radiographs more financially accessible for patients and reduces administrative burden for practices.
The cost-effectiveness extends beyond equipment and operational expenses. Staff training requirements for conventional radiographs are minimal compared to CBCT systems. Most dental assistants can become proficient in taking standard X-rays within weeks, while CBCT operation requires more extensive training and ongoing education. This translates to lower training costs and faster integration of new team members.
Quick acquisition time for efficient patient throughput
Speed matters in modern dental practice, and conventional radiographs excel in rapid image acquisition. A typical bitewing series takes less than 5 minutes to complete, while a full mouth series can be finished in 10-15 minutes. This efficiency allows practices to maintain smooth scheduling and minimize patient waiting times.
Digital conventional radiographs appear on the monitor within seconds of exposure, enabling immediate review and discussion with patients. This instant feedback loop enhances patient communication and allows for real-time treatment planning adjustments. Patients appreciate seeing their images immediately and understanding their oral health status without delays.
The streamlined workflow of conventional radiography fits seamlessly into busy practice schedules. Unlike CBCT scans that may require 20-40 minutes from patient positioning to image reconstruction, standard X-rays integrate effortlessly into routine appointments. This time efficiency means practitioners can see more patients per day while maintaining high-quality care standards.
Patient positioning for conventional radiographs is straightforward and comfortable for most individuals. The familiar bite-wing holders and positioning devices allow for quick, reproducible images without the claustrophobic concerns some patients experience with CBCT machines. This ease of positioning is particularly beneficial for anxious patients, children, and individuals with mobility limitations.
The rapid acquisition time also reduces motion artifacts that can compromise image quality. Since conventional X-ray exposures are measured in milliseconds, patient movement during the brief exposure time rarely affects diagnostic quality. This reliability means fewer retakes and less radiation exposure for patients.
For emergency situations, conventional radiographs provide immediate diagnostic information when time is critical. A periapical X-ray can quickly confirm a suspected root fracture or periapical pathology, allowing for prompt treatment decisions. This rapid diagnostic capability is invaluable in urgent care scenarios where every minute counts.
Excellent for detecting common dental pathologies
Conventional radiographs demonstrate exceptional diagnostic accuracy for the vast majority of dental pathologies encountered in daily practice. These proven imaging modalities excel at detecting interproximal caries, periodontal bone loss, periapical pathology, and restoration problems with reliability that has been validated through decades of clinical use.
Interproximal caries detection represents one of the strongest applications for bitewing radiographs. Studies consistently show that bitewing X-rays can detect proximal caries lesions earlier than clinical examination alone, often identifying decay before it becomes clinically visible. The contrast resolution of modern digital sensors allows practitioners to distinguish between enamel and dentin caries, enabling appropriate treatment planning based on lesion depth.
Periodontal assessment through conventional radiographs provides essential information about bone levels and patterns of bone loss. Bitewing and periapical images clearly demonstrate the alveolar crest height, interdental bone levels, and furcation involvement in multi-rooted teeth. This information guides periodontal treatment planning and allows for accurate monitoring of disease progression over time.
Periapical pathology shows characteristic radiolucent patterns on conventional radiographs that experienced practitioners can readily identify. Whether dealing with acute apical periodontitis, chronic periapical lesions, or root resorption, periapical X-rays provide the diagnostic clarity needed for endodontic treatment decisions. The high spatial resolution of conventional imaging allows for precise evaluation of root canal anatomy and treatment outcomes.
Restoration evaluation benefits tremendously from conventional radiographic assessment. Bitewing images reveal marginal integrity, secondary caries beneath restorations, and overhang presence with excellent detail. This diagnostic capability helps practitioners determine when restorations need replacement and guides material selection for optimal longevity.
Orthodontic treatment planning relies heavily on conventional radiographs for initial assessment and progress monitoring. Panoramic radiographs provide comprehensive views of tooth development, eruption patterns, and potential impactions. Cephalometric radiographs offer standardized measurements for growth assessment and treatment planning in orthodontic cases.
| Pathology Type | Conventional X-ray Sensitivity | Primary Imaging Choice |
|---|---|---|
| Interproximal Caries | 85-95% | Bitewing radiographs |
| Periodontal Disease | 90-95% | Bitewing/Periapical |
| Periapical Pathology | 80-90% | Periapical radiographs |
| Restoration Problems | 85-95% | Bitewing radiographs |
| Tooth Development | 95-100% | Panoramic radiographs |
The diagnostic confidence provided by conventional radiographs for common pathologies makes them indispensable tools for general dentistry. The ability to detect, monitor, and treatment plan for the majority of dental conditions using cost-effective, rapid imaging keeps conventional radiographs at the center of dental practice workflows.
Conventional radiographs also excel in follow-up care and monitoring treatment outcomes. Serial radiographs allow practitioners to track healing responses, monitor bone regeneration, and assess treatment success over time. This longitudinal assessment capability is particularly valuable for endodontic therapy, periodontal treatment, and implant healing evaluation.
The widespread familiarity of dental professionals with conventional radiographic interpretation creates additional diagnostic value. Decades of education and clinical experience have established standardized interpretation criteria that promote consistent, reliable diagnoses across different practitioners and practice settings. This collective expertise base supports evidence-based treatment decisions and reduces diagnostic uncertainty.
Quality assurance for conventional radiographs is well-established and straightforward to implement. Standard protocols for exposure settings, processing parameters, and image evaluation help maintain consistent diagnostic quality. This reliability gives practitioners confidence in their diagnostic decisions and supports defensible treatment planning documentation.
The combination of cost-effectiveness, efficiency, and diagnostic accuracy makes conventional radiographs the optimal imaging choice for routine dental care. While advanced imaging technologies like CBCT have their place in complex cases, the fundamental value proposition of conventional radiography continues to serve the daily needs of dental practice exceptionally well. Understanding when conventional radiographs provide sufficient diagnostic information allows practitioners to use their imaging resources wisely while delivering excellent patient care.
Clinical Scenarios Where CBCT Delivers Superior Results
Complex Endodontic Cases Requiring Precise Root Canal Assessment
When dealing with challenging root canal treatments, CBCT imaging transforms how practitioners approach endodontic diagnosis and treatment planning. Traditional periapical radiographs provide valuable information, but they compress three-dimensional anatomy into a two-dimensional image, often masking critical details that can make or break treatment success.
Root Anatomy Visualization
CBCT excels in revealing complex root canal anatomy that conventional radiographs simply cannot capture. Curved canals, C-shaped configurations, and accessory canals become clearly visible in three dimensions. This detailed visualization is particularly valuable in posterior teeth, where anatomical variations are common and can significantly impact treatment outcomes. The technology allows practitioners to identify MB2 canals in maxillary molars with remarkable accuracy, reducing the likelihood of missed canals that could lead to endodontic failure.
The ability to visualize root canal systems from multiple angles provides unprecedented insight into canal morphology. Practitioners can rotate and manipulate the CBCT data to understand exactly how canals branch, merge, and communicate with each other. This comprehensive view enables more predictable cleaning and shaping protocols, ultimately improving treatment success rates.
Periapical Pathology Assessment
CBCT imaging reveals the true extent of periapical lesions with remarkable precision. Unlike conventional radiographs that may underestimate lesion size due to cortical bone overlay, CBCT provides accurate three-dimensional measurements of pathological changes. This information proves invaluable for treatment planning, prognosis determination, and monitoring healing progress over time.
The technology’s ability to detect early periapical changes before they become visible on conventional radiographs represents a significant diagnostic advantage. Small osteolytic lesions that might go unnoticed on periapical films become clearly apparent on CBCT scans, enabling earlier intervention and potentially better treatment outcomes.
Retreatment Planning
Endodontic retreatment cases particularly benefit from CBCT assessment. The technology reveals the exact location and extent of previous obturation materials, separated instruments, and perforation sites. This detailed information allows practitioners to develop precise treatment strategies, anticipate potential complications, and communicate realistic expectations to patients.
Oral Surgery Planning for Impacted Teeth Extraction
Surgical extraction of impacted teeth, particularly third molars, represents one of the most compelling applications for CBCT imaging. The three-dimensional visualization capabilities provide surgical insights that conventional panoramic radiographs cannot match, leading to safer procedures and better patient outcomes.
Anatomical Relationship Assessment
CBCT imaging provides detailed visualization of the spatial relationship between impacted teeth and critical anatomical structures. The proximity of mandibular third molars to the inferior alveolar nerve canal becomes clearly apparent, allowing surgeons to assess risk levels and modify surgical approaches accordingly. Cross-sectional views reveal whether the nerve canal is positioned lingually, buccally, or interradicular to the impacted tooth, information that proves crucial for surgical planning.
The technology also excels in evaluating the relationship between maxillary third molars and the maxillary sinus. CBCT clearly shows whether extraction might result in oroantral communication and helps surgeons prepare appropriate treatment protocols to manage this potential complication.
Root Morphology and Bone Density Evaluation
Understanding root configuration before surgery enables better instrument selection and surgical approach planning. CBCT reveals root dilacerations, fusions, and unusual morphologies that could complicate extraction procedures. The ability to visualize root anatomy in three dimensions helps surgeons anticipate the need for sectioning techniques and plan appropriate flap designs.
Bone density assessment through CBCT imaging provides valuable information about healing potential and surgical difficulty. Dense cortical bone patterns may indicate the need for more aggressive bone removal techniques, while areas of decreased bone density might suggest altered healing patterns or pathological conditions requiring attention.
Surgical Access Planning
The detailed anatomical information provided by CBCT enables precise surgical access planning. Surgeons can determine optimal flap design, identify the best approach angle for tooth removal, and anticipate bone removal requirements. This level of planning reduces surgical time, minimizes tissue trauma, and improves patient comfort during recovery.
Periodontal Bone Loss Evaluation and Implant Site Analysis
CBCT imaging revolutionizes periodontal diagnosis and implant treatment planning by providing accurate three-dimensional assessment of bone architecture and pathological changes. The technology’s ability to visualize both hard and soft tissue relationships offers comprehensive information for treatment planning.
Precise Bone Level Assessment
Unlike conventional radiographs that may mask bone loss due to overlapping structures, CBCT provides accurate measurements of alveolar bone levels around teeth. The technology reveals both horizontal and vertical bone loss patterns with remarkable precision, enabling more accurate staging and grading of periodontal conditions. This detailed assessment proves particularly valuable in complex cases where conventional radiographic interpretation might be challenging.
The ability to evaluate bone architecture in three dimensions helps practitioners understand the extent of furcation involvement in multi-rooted teeth. CBCT clearly shows the degree of bone loss in furcation areas, information that directly impacts treatment planning and prognosis determination.
Implant Site Assessment
CBCT imaging has become the gold standard for implant site evaluation, providing essential information about bone volume, density, and anatomical limitations. The technology enables precise measurement of available bone height and width, allowing practitioners to select appropriate implant dimensions and plan optimal placement positions.
Anatomical Structure Identification
Critical anatomical structures like the inferior alveolar nerve, mental foramen, and maxillary sinus become clearly visible on CBCT scans. This visualization enables safe implant placement by helping practitioners maintain appropriate safety margins from vital structures. The ability to trace nerve pathways and assess sinus pneumatization patterns reduces the risk of surgical complications and improves treatment predictability.
Bone Quality Evaluation
CBCT provides valuable information about bone density and quality throughout the implant site. Practitioners can identify areas of dense cortical bone that might require modified drilling protocols, as well as regions of poor bone quality that could affect implant stability. This information enables appropriate treatment modifications and helps set realistic expectations for osseointegration timelines.
TMJ Disorders Requiring Detailed Joint Examination
Temporomandibular joint evaluation represents another area where CBCT imaging provides significant diagnostic advantages over conventional radiographic techniques. The complex anatomy of the TMJ and its three-dimensional nature make CBCT particularly well-suited for comprehensive joint assessment.
Osseous Change Detection
CBCT excels in detecting subtle osseous changes in TMJ components that might be missed on conventional radiographs. Early signs of osteoarthritis, including surface irregularities, osteophyte formation, and subcortical sclerosis, become clearly visible. The technology’s high resolution enables detection of these changes before they become apparent on standard imaging, potentially allowing for earlier intervention.
The ability to evaluate both condylar and temporal components simultaneously provides comprehensive assessment of joint pathology. CBCT clearly shows erosive changes, flattening, and remodeling patterns that help practitioners understand disease progression and treatment responses.
Joint Space Evaluation
CBCT provides detailed visualization of joint space dimensions and irregularities that conventional radiographs cannot accurately assess. The technology reveals areas of joint space narrowing, which may indicate disc displacement or degenerative changes. This information proves valuable for treatment planning and monitoring therapy effectiveness over time.
Condylar Position Assessment
The three-dimensional nature of CBCT imaging enables precise evaluation of condylar position within the glenoid fossa. Practitioners can assess whether condyles are positioned concentrically or if there are signs of displacement or malposition. This information proves crucial for understanding TMJ dysfunction and planning appropriate treatment interventions.
Airway Assessment for Sleep Apnea Treatment Planning
CBCT imaging provides comprehensive three-dimensional assessment of the upper airway, offering valuable information for sleep apnea diagnosis and treatment planning. The technology’s ability to visualize the entire airway from the nasal cavity to the hypopharynx makes it particularly useful for identifying anatomical factors contributing to sleep-disordered breathing.
Airway Volume Measurement
CBCT enables precise measurement of airway volumes at different anatomical levels, providing quantitative data about potential restriction sites. The technology can identify areas of narrowing in the nasal cavity, nasopharynx, oropharynx, and hypopharynx. This detailed volumetric analysis helps practitioners understand the severity and location of airway compromise.
The ability to measure cross-sectional areas at multiple levels provides comprehensive assessment of airway patency. Practitioners can identify the most constricted areas and plan treatment interventions accordingly, whether through surgical modification, orthodontic expansion, or oral appliance therapy.
Skeletal and Soft Tissue Evaluation
CBCT assessment reveals both skeletal and soft tissue factors contributing to airway restriction. Skeletal features like maxillary constriction, mandibular deficiency, and vertical facial patterns become clearly apparent. Soft tissue structures including tongue position, soft palate configuration, and pharyngeal wall thickness can be evaluated in relation to airway patency.
This comprehensive evaluation enables practitioners to identify multiple contributing factors and develop integrated treatment approaches. The three-dimensional visualization helps in planning combined orthodontic, surgical, and appliance therapies for optimal treatment outcomes.
Treatment Planning and Monitoring
CBCT imaging proves valuable for both treatment planning and outcome monitoring in airway therapy. Pre-treatment scans establish baseline measurements and identify target areas for intervention. Post-treatment imaging can objectively demonstrate airway volume changes and treatment effectiveness.
The technology enables precise planning of surgical procedures like maxillomandibular advancement or soft tissue modifications. Practitioners can simulate treatment outcomes and optimize surgical planning to achieve desired airway improvements while maintaining facial esthetics and function.
When Conventional Radiographs Remain the Optimal Choice
Routine Caries Detection and Monitoring
Conventional radiographs remain the gold standard for detecting and monitoring dental caries in clinical practice. The superior contrast resolution of traditional X-rays makes them exceptionally effective at revealing the subtle density changes that indicate early tooth decay. When examining interproximal surfaces, bitewing radiographs provide unmatched clarity in distinguishing between healthy enamel and demineralized tissue.
The radiation dose for conventional radiographs is significantly lower than CBCT scans, making them ideal for routine screening procedures. A typical bitewing series exposes patients to approximately 0.005 millisieverts (mSv) of radiation, compared to 0.1-0.5 mSv for a CBCT scan. This 10-100 fold difference becomes particularly important when considering the frequency of caries screening appointments.
Digital conventional radiographs offer immediate image availability and enhanced diagnostic capabilities through software tools like histogram equalization and edge enhancement. These features allow practitioners to identify incipient lesions that might not yet be clinically visible. The ability to adjust contrast and brightness settings helps differentiate between various stages of caries progression without requiring additional radiation exposure.
Advantages of conventional radiographs for caries detection:
- Exceptional contrast resolution for detecting demineralization
- Minimal radiation exposure suitable for routine use
- Cost-effective imaging solution
- Rapid acquisition and processing
- Standardized positioning for consistent monitoring
- Well-established interpretation criteria
The systematic approach to caries monitoring relies heavily on standardized radiographic techniques that conventional X-rays provide. Bitewing radiographs taken at consistent angles and positions allow for accurate comparison between visits, enabling practitioners to track lesion progression or regression over time. This reproducibility is essential for evidence-based treatment planning and insurance documentation.
Conventional radiographs excel at detecting secondary caries around existing restorations, where the metallic interfaces can create artifacts in CBCT imaging. The beam hardening effects common in cone beam CT can obscure important diagnostic information around crowns, fillings, and implants, making conventional X-rays the preferred choice for restoration monitoring.
Periodontal Screening and Maintenance Visits
Periodontal assessment represents another area where conventional radiographs demonstrate clear advantages over CBCT imaging. Intraoral periapical and bitewing radiographs provide the necessary detail for evaluating alveolar bone levels, detecting calculus deposits, and monitoring periodontal disease progression with minimal radiation exposure.
The high resolution of conventional digital sensors captures fine details of the periodontal ligament space, lamina dura, and cortical bone boundaries that are essential for periodontal diagnosis. These structures appear with greater clarity and contrast in conventional radiographs compared to CBCT reconstructions, where partial volume effects can blur important anatomical landmarks.
Key benefits for periodontal applications:
- Superior bone level assessment
- Clear visualization of periodontal ligament space
- Detailed furcation involvement evaluation
- Minimal radiation for routine monitoring
- Cost-effective for frequent recall appointments
- Established diagnostic criteria and treatment protocols
Conventional radiographs allow for precise measurement of bone loss using standardized reference points. The crown-to-root ratio calculations, percentage of bone loss determinations, and furcation classifications all rely on the dimensional accuracy that conventional X-rays provide. The parallel technique used in periapical radiography ensures consistent magnification factors for reliable measurements.
During maintenance visits, the ability to compare current radiographs with previous images is crucial for monitoring treatment outcomes and disease stability. Conventional radiographs taken with standardized positioning devices ensure reproducible geometry that enables accurate comparison over time. This consistency is particularly important for insurance documentation and medicolegal purposes.
The speed of conventional radiographic procedures fits well with typical hygiene appointment schedules. Patients can complete their cleaning appointment with minimal interruption, and the immediate image availability allows for real-time treatment planning discussions. CBCT scans require significantly more time for both acquisition and interpretation, making them impractical for routine maintenance visits.
Conventional radiographs also excel at detecting subgingival calculus deposits that may not be clinically apparent during probing. The radiopaque appearance of calcified deposits contrasts sharply with the surrounding tooth structure and soft tissues, providing hygienists and dentists with valuable information for thorough debridement procedures.
Pediatric Dentistry Applications with Radiation Concerns
Pediatric dental care demands special consideration for radiation exposure, making conventional radiographs the preferred imaging modality for young patients. The developing tissues in children are more radiosensitive than adult tissues, requiring practitioners to carefully balance diagnostic benefits with potential radiation risks.
The ALARA principle (As Low As Reasonably Achievable) is particularly important in pediatric dentistry. Conventional digital radiographs can reduce radiation exposure by up to 80% compared to traditional film, while CBCT scans expose children to radiation doses equivalent to several months of natural background radiation. This significant difference makes conventional X-rays the responsible choice for routine pediatric procedures.
Pediatric-specific advantages:
- Minimal radiation exposure for developing tissues
- Faster acquisition reduces motion artifacts
- Smaller sensors accommodate limited mouth opening
- Less intimidating equipment for anxious children
- Age-appropriate radiation safety protocols
- Cost-effective for frequent monitoring needs
The rapid acquisition time of conventional radiographs is particularly beneficial when working with children who have difficulty remaining still. A typical bitewing or periapical image requires only 0.1-0.2 seconds of exposure time, compared to 10-20 seconds for CBCT scans. This time difference significantly reduces the likelihood of motion artifacts that can compromise diagnostic quality.
Conventional radiographs are well-suited for monitoring the mixed dentition period, where practitioners need to track primary tooth resorption and permanent tooth development. The high contrast resolution allows for clear visualization of developing tooth buds, root resorption patterns, and space management issues that are common concerns in pediatric dentistry.
The smaller sensor sizes available for conventional digital radiography accommodate the limited mouth opening capacity of young children. Size 0 and 1 sensors can capture diagnostic images without causing discomfort or triggering gag reflexes that might interfere with CBCT positioning requirements.
Conventional radiographs also support established pediatric treatment protocols for common conditions like early childhood caries, ectopic eruption, and space loss evaluation. The diagnostic criteria for these conditions have been developed and validated using conventional radiographic techniques, providing practitioners with confidence in their treatment planning decisions.
The psychological impact of imaging procedures should not be overlooked in pediatric dentistry. Conventional radiographic equipment appears less intimidating to children compared to the larger CBCT machines that require patients to remain motionless in a standing or seated position for extended periods. The familiar appearance of intraoral sensors and quick procedure completion helps maintain child cooperation and reduces anxiety.
Parental concerns about radiation exposure are also more easily addressed with conventional radiographs. The dramatically lower radiation doses and well-established safety record of conventional X-rays provide reassurance to parents who may be hesitant about dental imaging procedures. Clear communication about radiation levels equivalent to natural background exposure helps build trust and treatment acceptance.
Emergency situations in pediatric dentistry often require immediate imaging for trauma assessment or acute pain evaluation. Conventional radiographs can be obtained quickly without scheduling delays or extensive positioning requirements, allowing for prompt diagnosis and treatment of urgent conditions. The immediate availability of images enables real-time clinical decision-making that may be critical for preserving developing teeth and supporting structures.
Cost-Benefit Analysis for Different Practice Settings
Making Evidence-Based Imaging Decisions
Patient-specific factors influencing modality selection
Making smart imaging decisions starts with looking closely at each patient’s unique situation. Your patient’s age plays a huge role in this choice. Younger patients, especially children and teens, have developing tissues that are more sensitive to radiation. This means you’ll want to be extra careful about radiation exposure and lean toward conventional radiographs when they can provide the diagnostic information you need.
The patient’s medical history tells you a lot about which imaging approach makes sense. Someone with a history of cancer, particularly head and neck cancers, might need the detailed views that CBCT provides to check for recurrence or monitor treatment effects. On the flip side, a healthy patient coming in for routine preventive care probably doesn’t need the comprehensive imaging that CBCT offers.
Pregnancy status completely changes your imaging strategy. Pregnant patients should avoid CBCT except in true emergencies where the diagnostic information is absolutely critical for immediate treatment. Conventional radiographs with proper shielding remain the safer choice during pregnancy.
The patient’s cooperation level matters more than you might think. CBCT requires patients to remain perfectly still for longer periods compared to conventional X-rays. Someone with Parkinson’s disease, severe anxiety, or claustrophobia might not be able to handle the CBCT scanning process. Pediatric patients often struggle with staying still long enough for quality CBCT images.
Previous imaging results guide your next steps. If recent conventional radiographs show suspicious areas that need clearer definition, CBCT becomes the logical next step. But if previous CBCT scans are recent and showed normal findings, you probably don’t need another high-dose imaging session for routine follow-up.
Patient symptoms and chief complaints directly influence your imaging choice. Sharp, localized pain that doesn’t respond to initial treatment might warrant CBCT to rule out vertical root fractures or complex periapical pathology that conventional films might miss. However, generalized discomfort or routine dental pain often gets diagnosed effectively with conventional radiographs.
The complexity of the patient’s dental history affects your decision too. Someone with extensive restorative work, multiple endodontic treatments, or a history of trauma might benefit from the three-dimensional view that CBCT provides. These complex cases often have overlapping structures or unusual anatomy that conventional films can’t fully capture.
Financial considerations can’t be ignored when making patient-specific decisions. While you want to provide the best care possible, you also need to consider what the patient can afford. CBCT costs significantly more than conventional radiographs, and not all insurance plans cover the additional expense. Having an honest conversation with patients about the benefits versus costs helps them make informed decisions about their care.
Diagnostic yield optimization strategies
Getting the most diagnostic information from your imaging choices requires strategic thinking about what you’re trying to accomplish. Start by clearly defining your diagnostic goals before selecting an imaging modality. Are you screening for caries, evaluating bone levels, planning implant placement, or investigating unexplained symptoms? Your specific objective should drive your imaging choice.
Timing your imaging appropriately maximizes diagnostic value. Don’t order CBCT during acute infections when swelling and inflammation might obscure anatomical details. Wait for acute conditions to resolve before using advanced imaging for comprehensive evaluation. Conventional radiographs often work better during acute phases because they provide the essential information you need without the added complexity.
Combining imaging modalities strategically increases your diagnostic accuracy. Start with conventional radiographs for initial assessment, then move to CBCT only when the conventional films raise questions that need three-dimensional clarification. This stepped approach prevents over-imaging while ensuring you don’t miss important details.
Understanding the limitations of each modality helps you set realistic expectations. Conventional radiographs excel at showing caries, bone levels, and basic pathology, but they struggle with overlapping structures and complex anatomy. CBCT provides excellent bone detail and spatial relationships but might not show soft tissue pathology as clearly as other imaging methods.
Image quality factors significantly impact diagnostic yield. Poor positioning, patient movement, or improper exposure settings can render even the most advanced imaging useless. Make sure your team knows how to optimize image acquisition for both conventional and CBCT systems. Regular quality assurance checks keep your equipment performing at peak levels.
Developing systematic interpretation protocols improves diagnostic consistency. Create checklists for reviewing conventional radiographs and CBCT scans so you don’t miss subtle findings. Train your entire team to recognize when images need retaking due to poor quality or positioning errors.
Correlation with clinical findings enhances diagnostic accuracy. Images should always be interpreted alongside clinical examination findings, patient symptoms, and medical history. Don’t rely solely on imaging to make diagnoses – use it as one piece of the diagnostic puzzle.
Consider the diagnostic confidence level you need for treatment planning. Some procedures require absolute certainty about anatomical structures and pathology, making CBCT the clear choice. Other treatments can proceed safely based on conventional radiographic findings combined with clinical judgment.
Documentation of your decision-making process protects both you and your patients. Record why you chose specific imaging modalities and how the results influenced your treatment planning. This documentation proves valuable for insurance purposes and medicolegal protection.
Radiation safety principles guiding clinical choices
Radiation protection principles must guide every imaging decision you make. The ALARA principle – As Low As Reasonably Achievable – forms the foundation of responsible imaging practices. This means using the lowest radiation dose that still provides the diagnostic information you need for patient care.
Understanding radiation dose comparisons between modalities helps you make informed choices. A single periapical radiograph delivers approximately 5 microsieverts of radiation, while a full-mouth series ranges from 35-170 microsieverts. CBCT scans typically range from 30-600 microsieverts depending on the field of view and acquisition parameters. These numbers put the radiation exposure in perspective when weighing benefits against risks.
Field of view selection in CBCT dramatically affects radiation exposure. Large field of view scans expose significantly more tissue to radiation than small, focused scans. Always use the smallest field of view that captures the anatomy you need to evaluate. A small field CBCT for evaluating one tooth delivers much less radiation than a full head scan.
Patient shielding techniques reduce unnecessary radiation exposure during both conventional and CBCT imaging. Lead aprons and thyroid collars remain standard protection for conventional radiographs. CBCT requires special considerations since traditional lead aprons might interfere with the rotating scanner, but thyroid shielding remains important.
Age-adjusted imaging protocols recognize that children are more sensitive to radiation than adults. Use faster film speeds or digital sensors with lower radiation requirements for pediatric patients. Consider longer intervals between routine imaging for young patients, and always justify imaging with specific diagnostic needs rather than following rigid schedules.
Quality assurance programs minimize radiation exposure while maximizing image quality. Regular equipment calibration, proper maintenance, and technique optimization ensure you’re not exposing patients to unnecessary radiation due to equipment problems or poor technique. Retakes due to poor image quality double the radiation exposure for no diagnostic benefit.
Staff training in radiation safety protects both patients and team members. Everyone who operates imaging equipment should understand radiation physics, safety protocols, and optimization techniques. Regular continuing education keeps your team current with evolving best practices in radiation safety.
Risk-benefit analysis becomes especially important for patients who need frequent imaging. Someone undergoing orthodontic treatment, endodontic therapy, or implant planning might accumulate significant radiation exposure over time. Balance the diagnostic benefits against cumulative radiation risks, and consider extending intervals between imaging sessions when clinically appropriate.
Pregnancy considerations require special attention to radiation safety. Always ask about pregnancy status before any imaging procedure. When imaging pregnant patients is absolutely necessary, use the fastest image acquisition methods possible and ensure proper shielding of the abdomen and pelvis.
Alternative diagnostic methods should be considered when appropriate. Clinical examination, pulp testing, percussion, palpation, and other clinical diagnostic tools might provide sufficient information without radiation exposure. Don’t automatically reach for imaging when clinical methods can answer your diagnostic questions.
Equipment selection impacts radiation exposure. Modern digital sensors and CBCT units with advanced dose reduction features deliver less radiation than older equipment. Investing in current technology benefits both patient safety and diagnostic quality.
Patient communication about radiation risks and benefits builds trust and ensures informed consent. Explain why you’re recommending specific imaging, what information you expect to gain, and how it will influence treatment. Most patients appreciate understanding the reasoning behind imaging recommendations.
Regular review of imaging protocols keeps your practice aligned with current safety standards. Professional organizations regularly update guidelines based on new research and technology developments. Stay current with these recommendations and adjust your protocols accordingly.
Documentation of radiation safety measures provides important medicolegal protection. Record the clinical justification for imaging, the specific technique used, and any special precautions taken. This documentation demonstrates your commitment to responsible imaging practices.
The choice between CBCT and conventional radiographs doesn’t have to be overwhelming when you understand what each technology brings to the table. CBCT shines in complex cases requiring three-dimensional visualization, detailed bone assessment, and precise treatment planning, while conventional radiographs continue to excel in routine diagnostics, screening procedures, and situations where radiation exposure needs to stay minimal. Your practice setting, patient demographics, and case complexity should drive these imaging decisions rather than simply defaulting to the newest technology.
Smart imaging choices come down to matching the right tool to the specific clinical need while keeping costs and patient safety in mind. Start by evaluating your most common cases and identifying where each imaging type would add the most value. Remember that the best imaging decision is one that provides the necessary diagnostic information efficiently and safely, helping you deliver better patient care without unnecessary complexity or expense.
